Fighting mislabeling and fish fraud with science-based systems

In 2016, global per capita fish consumption hit 20kg for the first time. In 2019, the trend had not stopped and consumption reached 20.9kg, setting a new record.
For the Food and Agriculture Organization (FAO), the increase in per capita consumption of fish is the result of the development of aquaculture and of a general reduction of waste: in the 60s, 67% of fish was eaten by humans (the rest went to the animals), while today we eat almost 90% of it.
Although many marine species are still overfished and therefore at risk, the fact that fish consumption is increasing at a global scale and that a good part of it comes from aquaculture, must certainly be taken as good news: fish has a more sustainable footprint of livestock farms, that is for sure. On the other hand, the increased demand for fish, exposes the sector to fraudulent activities aimed to maximize profits to the detriment of consumers.
The numbers of fish fraud
In a report published by FAO, the fishing and aquaculture industries were recognized as especially vulnerable to food fraud. Fish fraud – which involves mislabeling, fish substitution, fraudulent increase in fish weight – occurs along the entire supply chain.
The most common type of fraud is certainly fish mislabeling, which favors the practice of substituting some fish species with less valuable ones.
According to studies, in Europe, out of a total of 283 fish samples collected in 180 retail outlets of 23 countries, 26% of the samples were mislabeled and 31% of the outlets sold mislabeled fish.
Other studies found that in the US as many as 33% of the 1,215 samples taken in 21 union states were mislabeled; 44% of the outlets actually sold one species of fish instead of another.
A research, aimed at integrating the results of more than 200 articles on fish fraud in 55 countries, has revealed that an average of 20% of all fish sold in retail and in restaurants is mislabeled. When put in relation with the global increase in fish consumption, these numbers provide a good idea of the extent of the problem and the risks associated to it.
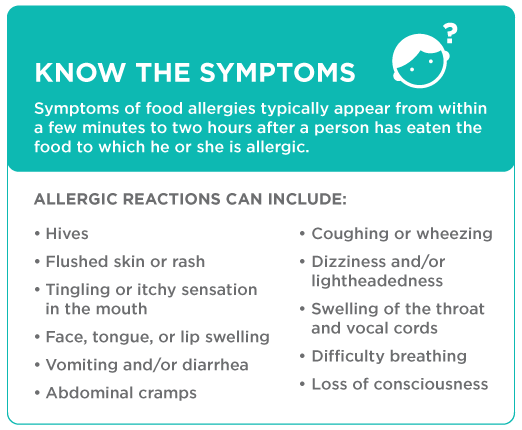
The immediate consequence of fish fraud is consumer deceiving. However, the effects on public health should not be underestimated: public health is at risk when, for example, toxic species replace non-toxic ones or when fish coming from polluted waterways is passed off as marine. The impacts of food fraud include loss of consumer confidence in both the food industry and in the effectiveness of government food control programs.
Tackling the problem
Fish fraud is a complex issue that requires the strengthening of control policies and the development of effective science-based tools and systems that can ensure the fish traceability and authenticity.
The fight against fraudulent practices in the fishing sector has entered the agenda of many political decision-makers. In Europe, EIT Food promoted a project aimed at developing an end-to-end electronic system for the analysis and traceability of fish along each step of the supply chain. Through a portable NIR spectrometer, it is now possible to perform non-destructive analysis in order to classify the species and provide information on the composition of the fish, measuring parameters such as fat, protein, humidity and spoilage. The system, which is based on an AI engine running in the cloud, is also able to measure the amount of water present in the fish and thus determine if fraudulent practices have been carried out or if the fish has been frozen.
The system integrates the analysis allowing the traceability of fish up to the origin. The information is recorded and protected via blockchain so as to provide an additional tool for the control and prevention of mislabeling.
Tackling fish fraud will not be an easy task. While the problem has been investigated in developed countries, there is a lack of information about fish fraud in developing countries. As policy makers started to include a science-based approach to the question, the fish supply chain also need to integrate its control systems to take account of risks of fraud. The goal is to ensure the quality of food on the market and give consumers the opportunity to make informed and more sustainable choices, ultimately gaining their trust again.
References
https://oceana.org/sites/default/files/National_Seafood_Fraud_Testing_Results_Highlights_FINAL.pdf
http://www.fao.org/3/i8791en/I8791EN.pdf
https://www.bbc.com/news/science-environment-36716579
https://www.sciencedirect.com/science/article/abs/pii/S095671351830207X